A PUBLIC HEALTH PROBLEM – PART 2
The evidence we already have on the contribution of poor sleep on health outcomes for both immediate and far-reaching, makes it imperative that addressing sleep health is crucial for preventive and promotive health. Since the many health issues raised by sleep deprivations are multifaceted, proper care for these sufferers demands the services of an interdisciplinary team consisting of physicians specialized in sleep medicine and other health professionals, like physical therapists, with expertise in this area of care.
Patients who suffer from Obstructive Sleep Apnea (OSA) clearly benefit from the use of a continuous airway pressure (CPAP) machine every night to aid their sleep. Based on the coexisting medical conditions like coronary artery disease, diabetes, obesity, depression etc., care by other specialists may be necessary.
Physical therapists have been noticing that many of their consumers receiving physical therapy because of their neurologic (e.g. stroke, Parkinson’s Disease, spinal cord injuries) or orthopedic (e.g. neck and back problems, major bone surgeries) conditions are also suffering from chronic insufficient sleep. Some of them were already victims of a sleep disorder often undiagnosed and untreated. An equally important issue of this: poor sleep can exacerbate or perpetuate their symptoms or slow down their recovery, thus impacting the outcomes. This cannot be ignored. As such, PTs have an ethical obligation to integrate sleep health with rehabilitative, wellness and health promotion interventions.
Physical Therapy Approaches
Here is a brief overview of how physical therapy may prove helpful. In essence, the role of physical therapy in integrating sleep health in prevention, health promotion and wellness interventions involves three components as follows:
Assessing overall sleep health and screening the level of risk for sleep disorders. Based on the answers to one or two simple questions during the initial assessment like, “How well are you sleeping?” or, “How many hours of sleep do you typically get?” you may want to proceed to the use of a more elaborate questionnaire to get a realistic picture of the sleep health.
Referring individuals identified as at increased risk for a sleep disorder to appropriate health professionals for care. This can be a turning point for some patients.
Provide care as outlined below:
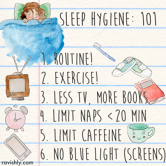
Sleep Hygiene Education
Instruct patients in ways to optimize sleep health by educating them about good sleep hygiene practices viz., the behaviors and environment that promote good sleep quality.
Institute a Suitable Therapeutic Exercise Program
Analytical studies indicate that acute and chronic exercise has a moderate positive benefit on sleep characteristics. Typically, recommended personalized exercises, including stretching and walking when possible, may be conducted, preferably in the morning or early afternoon; for many anytime of the day is good. Meditative movement including yoga, tai chi and qi gong are also good.
Positioning for Sleep and Addressing Bed Mobility to Facilitate Sleep
Since pain contributes to a poor quality of sleep, patients need to be educated in appropriate positioning in bed, based on their diagnosis and needed precautions. They need instruction to position themselves in a pain-free or pain-reduced position. Patients with impaired bed mobility and transfers need special consideration. They require training in both, to overcome these impairments, either by themselves or with or without mechanical or manual assistance.
Sleep health has now emerged as a sphere of successful outcomes. This is good news to millions of insomnia sufferers. Strategies and approaches outlined above can be of help. By being patient and persistent, you may be able to develop a new outlook on sleep and once again look eagerly to bedtime.